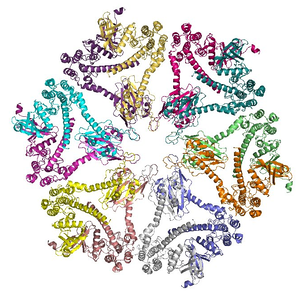
 Graphic model of an enzyme. Graphic model of an enzyme. The majority of us with cystic fibrosis or pancreatic insufficiency require pancreatic enzyme supplementation in order to digest our food. We need this because our pancreases may not produce enough pancreatic enzymes on our own due to a genetic mutation or other pancreatic malfunction. When this happens, the most common conventional intervention is prescription-strength digestive enzymes which are enteric coated. These work pretty well for the majority of us, but sometimes they don't work as well as they should for certain individuals. In this article I will explain what enteric-coated enzymes are, how they are designed to work, possible reasons why enteric-coated enzymes may not work for certain individuals, and a few options to address this problem.
3 Comments
 Artichoke leaf, a great digestive bitter. Artichoke leaf, a great digestive bitter. The long term use of stomach acid-lowering drugs such as proton pump inhibitors (PPIs) in the cystic fibrosis (CF) population, both adults and children, has been common for approximately 20 years. Today, more than 50% of CFers are using PPIs[i]. They are used for two main reasons: to treat gastroesophageal reflux and to improve supplemental pancreatic enzyme activation, particularly lipase. However, there are flaws in the reasoning for use of acid-lowering drugs in both of these situations. Firstly, the cause of reflux is not excessive secretion of stomach acid but dysfunction of upper gastrointestinal (GI) motility and secretions[ii], and further reducing gastric acidity with PPIs or antacids will further exacerbate reflux, causing a dependency on the drugs and worsening symptoms over time. Furthermore, the long-term use of PPIs has significant and far-reaching side effects that can negatively affect CF prognoses. Secondly, although several preliminary studies have demonstrated that the pH of the duodenum can be too low to provide the right environmental for supplemental pancreatic enzyme activation, it is not completely clear that bicarbonate secretion is inadequate in all cases, even if steatorrhea is present. A 2014 Cochrane Review of the use of PPIs in CF found that related clinical trials were not only biased, but showed zero or overall insignificant improvement in gastrointestinal symptoms[iii]. In fact, there may be other mechanisms at play within the duodenum that cause steatorrhea and contribute to low duodenal pH, namely inadequate bile secretion, possibly due to a diet low in bitter plant constituents. Here, I will discuss the issue of gastroesophageal reflux disease (GERD) in CF and the negative consequences of using PPIs to treat it. I will also discuss the many negative side effects of long term PPI use in the CF and general populations. In addition, I will discuss the low bicarbonate theory in its relationship to pancreatic enzyme activation, and how the use of PPIs may not be helpful in this situation. Lastly, I will discuss the role of bitter plant constituents in stimulating release of GI hormones and bile in the duodenum, their relationships to macronutrient absorption, and how the use of bitter tastants in the CF population may kill two birds with one stone: addressing GERD by correcting gastric sphincter function and GI secretions, and improving lipase activation by stimulating release of bile which emulsifies fats and stimulates bicarbonate secretion.  Digestive upset is a special kind of misery, and in cystic fibrosis and other digestive diseases it may be a common nuisance. Fortunately, herbal medicine is particularly effective in assisting people with these issues! All of our ancestors have been using medicinal herbs to address digestive distress for eons. Although conventional medicine has very few tools to assist us with gastrointestinal issues, especially with regards to chronic indigestion, there are many, many herbs which can help resolve GI symptoms including stomach aches, intestinal cramps, nausea, burping, constipation, loose stools and diarrhea, delayed gastric emptying, reflux, and more. In this article I will suggest a few herbs to use to address bloating and indigestion. There are so many medicinal herbs to choose from that I couldn't possibly discuss them all in one article, so I'll touch on a few that I use most frequently for myself and my clients.  In this article, originally published in AromaCulture Magazine in July, I discuss herbal and dietary support for CF children and adults. I discuss digestion, respiratory disease, liver support, and modulation of CFTR sodium chloride channels by natural means. Cystic fibrosis is an autosomal recessive genetic disease that leads to the malfunctioning of several organ systems but most especially impacts the lungs, sinuses, and digestion. It is the most common autosomal recessive genetic disorder (meaning that each parent must be a carrier of the genetic mutation) in people of Western European decent. There are approximately 30,000 people living with cystic fibrosis (CF) in the United States, and more than 70,000 people worldwide.  Artichoke leaf Artichoke leaf A friend of mine with CF who lives in South Africa has a history of severe gastroparesis (delayed gastric emptying) and low stomach acid, which (alongside her Crohn's, CFRD, and removal of her terminal ileum, ascending colon, and gallbladder years ago) has caused her significant digestive distress and inability to digest anything other than her extremely regimented liquid diet. For years Paula's gastroparesis has been so bad that if she doesn't eat precisely the right thing in precise quantities at precisely the right time of day, her stomach will not empty, which puts pressure on her diaphragm and lungs and can cause significant respiratory distress and vomiting. She is a great researcher and has tried many, many things to help this situation, but nothing had yet made a significant dent on these distressing symptoms (including multiple motility drugs). I've tried to strategize with Paula to figure out what was causing or had caused the issue, and secondly what do we do about it now. After a lot of trial and error, it seems we've found two things that have made a big difference in her life: lecithin and artichoke leaf (Cynara scolymus).  As a kid with CF, I was lucky in that I had heartburn rarely enough that regular use of antacids or PPIs (proton pump inhibitors) was not offered to me by my parents or doctors, so I never developed a dependence on them. But it seems such things are often suggested to CF patients as part of a standard CF routine. Due to a number of factors common in the CF lifestyle (poor diet, frequent antibiotic usage, stress, coughing, etc.) acid reflux, heartburn, and gastroesophageal reflux disease (GERD) are commonplace in the CF population. Yet mainstream medicine understands the problem entirely wrong, and so their standard treatment protocol ends up exacerbating the issue and causing more problems than you started with. I want to briefly discuss why antacids and PPIs are inappropriate for CF (and humans in general) and some alternatives to these pharmaceutical treatments for reflux. |
Author
Mica (they/he) is a clinical herbalist, nutritionist, researcher, and writer living in Abenaki territory (Vermont). *************************** Disclaimer: The content of this website and blog is for educational purposes only and should not be considered medical advice. The information provided here is not intended to replace medical care. Archives
July 2024
Categories
All
|
Photo from BotanikGuide
 RSS Feed
RSS Feed
