 Sunwort (St. John's Wort) which blooms around the summer solstice. Sunwort (St. John's Wort) which blooms around the summer solstice. In June 2023, I had two bouts of massive hemoptysis (coughing up blood) that eventually led to an emergency double lung transplant on July 5. I didn't know until it happened to me that massive bleeding could lead to lung transplant, so I want to take some time to discuss it here. The truth is, this is a scary story. I haven't wanted to share it with my readers because what happened to me was very, very unusual and probably won't happen to any of you. I don't like stoking fear in people who already have enough to be afraid of. However, I am usually of the opinion that knowing what the worst case scenario is can help us prepare and also feel less stressed in situations that are slightly less bad. So I’ll leave out most of the gory details here (which are honestly zombie movie worthy). In this article, I summarize what actually occurred, how I prepared for transplant, my experience receiving the transplant, and how I’m doing one year later.
2 Comments
 Red clover contains protective phytoestrogens. Red clover contains protective phytoestrogens. The sex hormone estrogen is implicated in hastening the progression of many chronic diseases. In particular, when compared to people with testes, menstruating people with ovaries are at higher risk of developing estrogen-dependent cancers[i], autoimmunity[ii][iii], and more rapid disease progression along with poorer prognosis in respiratory diseases such as asthma, chronic obstructive pulmonary disease (COPD), and cystic fibrosis[iv][v]. In different tissues estrogen has differing effects that include cell proliferation, immunomodulation, and stimulation of mucin secretion[vi][vii][viii]. Here I will briefly touch on what role estrogen is theorized to play in the pathogenesis of estrogen-dependent cancers and autoimmunity, but I will discuss in more depth the role that it plays in the disease progression of chronic respiratory diseases. Lastly, I will discuss the potential therapeutic effects of phytoestrogens on estrogen-related disease progression.  Back in 2014, I conducted a series of experiments inhaling essential oils through my nebulizer. I began these experiments at a time when I was due to use oral antibiotics again (a regular occurrence for me as a result of my chronic cystic fibrosis lung infections) but a snow storm prevented me from getting to the pharmacy. As they say, necessity if the mother of invention (or in this case, discovery)! Why Use Essential Oils? In 2014, I was in the midst of my clinical herbal training and had been learning about various medicinal plant constituents. In particular, the constituents called essential oils often have potent antimicrobial (antibacterial, antifungal, & antiviral) power. So I decided it was time to try an experiment with them to see if they could help me control my lung infections. I was very happy with the results and I'd love to share my findings with you!  Baikal skullcap Baikal skullcap Inflammation is a huge factor in the disease processes of cystic fibrosis. Some studies have shown that faulty CFTR mutations may directly result in inadequate quenching of radical oxygen species (ROS) or excessive release of other inflammatory compounds like cytokines [1,2]. In addition, our burden of chronic infection and gastrointestinal complications contribute secondary sources of inflammation. Chronic inflammation can lead to both localized and systemic issues. Localized inflammation in the lungs can lead to deficient and/or over-reactive immune responses, bronchitis, scarification and airway remodeling, allergies/asthma/hyper-reactive airway diseases, hemoptysis, pleurisy (inflammation of the pleura), and worsened infection. Localized inflammation in the gut can lead to reflux/GERD, esophagitis, gastritis, pancreatitis, gallbladder issues, liver issues, food sensitivities, malabsorption, autoimmune issues of the intestines, gut infections, general indigestion, and excessive mucus production in both the guts and the lungs (by vagal reflex). Systemic inflammation can cause insulin resistance, body pain, arthritis, achey joints and muscles, fever, fatigue, increased risk for autoimmunity, and increased risk for cardiovascular disease.  In this article, originally published in AromaCulture Magazine in July, I discuss herbal and dietary support for CF children and adults. I discuss digestion, respiratory disease, liver support, and modulation of CFTR sodium chloride channels by natural means. Cystic fibrosis is an autosomal recessive genetic disease that leads to the malfunctioning of several organ systems but most especially impacts the lungs, sinuses, and digestion. It is the most common autosomal recessive genetic disorder (meaning that each parent must be a carrier of the genetic mutation) in people of Western European decent. There are approximately 30,000 people living with cystic fibrosis (CF) in the United States, and more than 70,000 people worldwide.  For many years I've struggled with the choice of when to avoid antibiotics and what situations warrant their use. As a person with chronic lung infections related to cystic fibrosis, antibiotics have saved my life countless times, but in the last few years I've become dependent on them to function normally. Without antibiotics to control my chronic lung infections (MRSA and Pseudomonas), I often feel debilitating fatigue, get a daily fever, and cough lots and lots of mucus. While I've found many natural remedies over the years to reduce my infections, improve my immune system, and strengthen my overall health and digestion, the severity of my infections is such that I cannot avoid antibiotics completely. In general, there are no natural remedies that I know of that match the power of pharmaceutical antibiotics for use in many bacterial infections - and trust me, I've looked! As a result of my experiences both with conventional pharmaceuticals and natural medicine, my opinions about antibiotics have changed over the years. In the beginning of my healing journey and experimentation with natural medicines, I viewed antibiotics with skepticism and tried to avoid them as often as possible. I made the personal choice to suffer through many months of infection, fatigue, and heavy mucus loads in order to minimize my exposure to this class of drugs. I did this for two major reasons: minimizing the risk of developing antibiotic resistance, and mitigating the impact that excessive use of antibiotics has on the gut microbiome. For about four years, I chose to wait as long as possible between hospitalizations, and do without oral antibiotics for longer and longer periods of time. Upon reflection, I think avoiding antibiotics as often as I did was a mistake, and I wouldn't recommend people do what I did. I lost lung function during that period and developed some serious and irreversible lung damage. It's not clear whether or not this damage would have developed anyway, even if I had taken more antibiotics. I now believe that the cost-benefit analysis weighs out in favor of using antibiotics when appropriate. In the last year or so I have changed tactics and my health has benefited. Here, I will describe my experiences and review why I made these changes.  Turmeric root, Curcuma longa Turmeric root, Curcuma longa Since about 2013, a portion of the CF community has been experimenting with "the Combo", or the combination of curcumin plus genistein supplements to help modulate CFTR function. This intervention is proving to be very helpful for many people who try it, yet we're still in the beginning stages of our experimentation. The impacts of the Combo are somewhat mutation-specific, and the rate of digestive absorption of these herbs varies person to person, thus the dose must be deduced via personal experimentation. The Combo is a simple and safe intervention with few side effects and is relatively cheap (compared to pharmaceutical CFTR modulators like Kalydeco, which cost $300,000 a year!). Both of these supplements are made up of plant constituents (genistein from soy and curcumin from turmeric root), and as you know, I'm an herbalist and a believer in the healing power of plants.  On occasion one must do strange things in the name of science. Sometimes it's necessary to challenge a few taboos to find useful information. There's hardly a body part with more taboos attached to it than the bung-hole. Oh yes, my friend. I'm going there. Let us discuss that place that our culture chooses not to think about. The "deep space" of our body. The rectum. It's a pretty useful spot. Located in between the bowel and the anus, it is of course wonderfully useful for expelling feces. And because it is a highly vascularized area of tissue, it is also very useful for absorbing things into the bloodstream. Rectal suppositories of medicine have been used for centuries, and more recently it's come to my attention that essential oils can be administered systemically via this technique.  Thyme (Thymus vulgaris) Thyme (Thymus vulgaris) For an introduction to inhaling essential oils in general, click here. In mid-May I began inhaling Benchmark Thyme essential oil in my nebulizer. For two and a half weeks I inhaled 3 drops of the oil mixed with 3mL of normal saline and nebulized it twice a day. By the end of this 2.5 week trial period I noticed a significant improvement in my lung and overall health. Of the oils I have used so far, Benchmark Thyme (BT) is probably my single favorite. In the two weeks before starting BT I was inhaling a combo of eucalyptus and tea tree oils. Although these oils kept me from declining back to pre-essential oil levels, when I began using thyme I could notice a difference. My main lung bug is MRSA, and since BT is specifically formulated to target MRSA infections, I believe this is why it has been so effective for me. 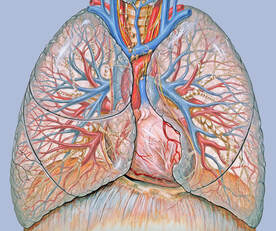 Coughing up blood ain't fun, and sometimes it can be kinda scary. I began to see blood in my sputum once in a while beginning in high school. Now it's a bit more frequent and in larger quantities, but I don't let it get me too worried anymore because I know how it works and what to do in an emergency. I thought I would talk about hemoptysis a little bit here, as it is something you might run into, and it can be scary for someone who is new to it. Some of these things can be worrying to think about, but ultimately the point of this post is to inform you of the possibilities so that you are prepared to do what needs to be done in these situations. By asking questions and learning as much as I could about this topic, I've faced my fears and eliminated the anxiety I used to have over coughing up blood. Now I know what to do and am unafraid. I hope this info can help you, too. |
Author
Mica (they/he) is a clinical herbalist, nutritionist, researcher, and writer living in Abenaki territory (Vermont). *************************** Disclaimer: The content of this website and blog is for educational purposes only and should not be considered medical advice. The information provided here is not intended to replace medical care. Archives
July 2024
Categories
All
|
Photo from BotanikGuide
 RSS Feed
RSS Feed
