 I recently learned about a fantastic organization that I want all CFers in the U.S. to know about: CF Bridge of Hope. Their mission is to "to improve the health of individuals with cystic fibrosis, and extend the same treatments that are available in the United States to those who live in resource-limited areas of the world." CF Bridge fully funds a 10 day trip to the U.S. for the patient and parent to get all necessary tests and to learn about CF care. They then go home with 1 year of all the meds they need! CF Bridge currently serves 60 patients from Pakistan, Ecuador, Tunisia, Algeria, Columbia, Libya, etc. I feel so privileged to live in a place where quality CF care and medications are accessible to me, but there are many CFers who live in places where this is not the case. For those of us in the Global North, I think it's very important to share resources and be in solidarity with others in the Global South without access to these life-saving treatments and medications. You can mail unused medications to a U.S. address which will get the meds to CFers in need abroad. I'm doing that this week because I have some extra CF meds I won't be using and I don't want them to go to waste! You can also donate money. Visit https://www.cfbridgeofhope.org/ to learn more.
0 Comments
 Sunwort (St. John's Wort) which blooms around the summer solstice. Sunwort (St. John's Wort) which blooms around the summer solstice. In June 2023, I had two bouts of massive hemoptysis (coughing up blood) that eventually led to an emergency double lung transplant on July 5. I didn't know until it happened to me that massive bleeding could lead to lung transplant, so I want to take some time to discuss it here. The truth is, this is a scary story. I haven't wanted to share it with my readers because what happened to me was very, very unusual and probably won't happen to any of you. I don't like stoking fear in people who already have enough to be afraid of. However, I am usually of the opinion that knowing what the worst case scenario is can help us prepare and also feel less stressed in situations that are slightly less bad. So I’ll leave out most of the gory details here (which are honestly zombie movie worthy). In this article, I summarize what actually occurred, how I prepared for transplant, my experience receiving the transplant, and how I’m doing one year later. After years of struggling with chronic – and dangerous – reactive hypoglycemia, I finally tried the keto diet and it’s changed my life forever. Reducing dietary carbohydrates to resolve chronic low blood sugar may seem counter-intuitive, but for people with dysregulated insulin production or insulin resistance, low-carbohydrate diets like the ketogenic diet may be the most effective choice for preventing hypoglycemic attacks. I struggled with chronic reactive hypoglycemia (low blood sugar after meals) for years until I started the keto diet in 2020. This change has been transformative for me and many others struggling with unstable blood sugar. In this article, I explain the science of why post-meal hypoglycemia occurs, what steps I’ve taken to prevent it from happening, and how I’ve made a ketogenic diet a sustainable choice for myself. If you’ve struggle with hypoglycemia and blood sugar imbalances like me, the ketogenic diet could be a great solution for reclaiming your health.
 In October 2020 I began a very successful experiment with the ketogenic diet to control my reactive hypoglycemia. I wrote this post in April 2021 outlining the initial phases of this experiment. Since then, a lot has changed, so I wanted to give an update on how it's working for me now. Even though I had been "keto" for a year and a half, I had been pretty loosey-goosey with my carb limits. As long as I stuck under 60g carbs/day I could see that I was producing a little bit of ketones (using a ketone meter) and this kept my glucose relatively stable. After a few months of keto, my A1c dropped dramatically from 6.2 down to 5.2. I'm holding steady now at around 5.3. But because I was a little lax with my carbs, especially between the end of 2021 and the beginning of 2022, I would regularly get hypoglycemic crashes once every couple of weeks which I required a rescue remedy (a half of a cube of maple sugar). So recently I've gotten much more strict with my carb intake, and the results have been excellent. My ketones are in optimal range almost all the time, my energy and digestion is great, and my blood sugar is in better control than ever before.  Homemade coconut milk. Homemade coconut milk. Hey friends. I wanted to write quickly about something I've been making regularly as a better alternative to animal milk and commercially-made plant milks: homemade coconut milk. I've been animal-milk-free for about nine years, and have switch between different plant milk alternatives, mostly hemp milk. However, there are several issues with these commercially available alternative milks: sustainability (where and how is the plant material grown, the energy and water used for that growth and processing, the waste involved in the packaging, and so on); hidden ingredients; not enough fat (for a CFer); and price. The best solution I've found to all these is to make your own milk, specifically from canned coconut milk. Yes, there are sustainability problems for a person in a northern climate to use a milk made from a tropical plant grown thousands of miles away, and the fossil fuels that transport depends on. There's no denying that. So a better alternative would be something like sunflower seeds, which grow in my bioregion. However, that requires some infrastructure that I don't have. Using canned coconut milk is a quick and easy solution and solves the issue of waste from milk containers. In addition, this milk alternative is very high in fat, which is great for CFers and others who need more nutrition. So here I'll give directions how to make it in addition to the nutrition facts. 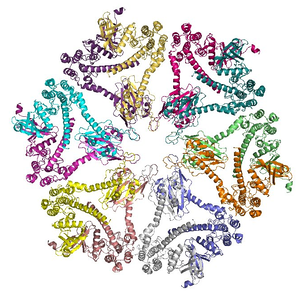 Graphic model of an enzyme. Graphic model of an enzyme. The majority of us with cystic fibrosis or pancreatic insufficiency require pancreatic enzyme supplementation in order to digest our food. We need this because our pancreases may not produce enough pancreatic enzymes on our own due to a genetic mutation or other pancreatic malfunction. When this happens, the most common conventional intervention is prescription-strength digestive enzymes which are enteric coated. These work pretty well for the majority of us, but sometimes they don't work as well as they should for certain individuals. In this article I will explain what enteric-coated enzymes are, how they are designed to work, possible reasons why enteric-coated enzymes may not work for certain individuals, and a few options to address this problem.  Why have gluten intolerances, food sensitivities, food allergies, and autoimmune diseases become so much more common in modern society? What are some natural, holistic ways to address these issues that can reduce the painful symptoms and heal the gut? In this article I discuss several factors in the development of gluten intolerance and food sensitivities, and offer a suggested protocol on how to address these problems and heal the gut with good nutrition, an elimination diet, herbal medicine, and probiotics to rebalance the gut microbiome and correct a leaky gut.  Stevia leaf Stevia leaf As a person struggling with CF-related diabetes, I've tried lots of things to balance my blood sugar over the years. It wasn't until 2020 when I discovered the ketogenic diet that my life really changed for the better and my blood sugar came under excellent control. Diet is the primary intervention for controlling most types of diabetes, but sometimes we may need medications and/or herbal medicines to assist with glucose control. I recently taught an in-depth class on holistic nutrition and herbal medicine for diabetes and blood sugar imbalances including CFRD, types I and II diabetes, metabolic syndrome, reactive hypoglycemia, and glucose intolerance (which you can check out here). I cover the topics of diet and herbs very comprehensively in that class, but in this article I'll mention briefly a few medicinal herbs that I have used and recommended to other diabetics to assist with blood sugar control.  Red clover contains protective phytoestrogens. Red clover contains protective phytoestrogens. The sex hormone estrogen is implicated in hastening the progression of many chronic diseases. In particular, when compared to people with testes, menstruating people with ovaries are at higher risk of developing estrogen-dependent cancers[i], autoimmunity[ii][iii], and more rapid disease progression along with poorer prognosis in respiratory diseases such as asthma, chronic obstructive pulmonary disease (COPD), and cystic fibrosis[iv][v]. In different tissues estrogen has differing effects that include cell proliferation, immunomodulation, and stimulation of mucin secretion[vi][vii][viii]. Here I will briefly touch on what role estrogen is theorized to play in the pathogenesis of estrogen-dependent cancers and autoimmunity, but I will discuss in more depth the role that it plays in the disease progression of chronic respiratory diseases. Lastly, I will discuss the potential therapeutic effects of phytoestrogens on estrogen-related disease progression.  Artichoke leaf, a great digestive bitter. Artichoke leaf, a great digestive bitter. The long term use of stomach acid-lowering drugs such as proton pump inhibitors (PPIs) in the cystic fibrosis (CF) population, both adults and children, has been common for approximately 20 years. Today, more than 50% of CFers are using PPIs[i]. They are used for two main reasons: to treat gastroesophageal reflux and to improve supplemental pancreatic enzyme activation, particularly lipase. However, there are flaws in the reasoning for use of acid-lowering drugs in both of these situations. Firstly, the cause of reflux is not excessive secretion of stomach acid but dysfunction of upper gastrointestinal (GI) motility and secretions[ii], and further reducing gastric acidity with PPIs or antacids will further exacerbate reflux, causing a dependency on the drugs and worsening symptoms over time. Furthermore, the long-term use of PPIs has significant and far-reaching side effects that can negatively affect CF prognoses. Secondly, although several preliminary studies have demonstrated that the pH of the duodenum can be too low to provide the right environmental for supplemental pancreatic enzyme activation, it is not completely clear that bicarbonate secretion is inadequate in all cases, even if steatorrhea is present. A 2014 Cochrane Review of the use of PPIs in CF found that related clinical trials were not only biased, but showed zero or overall insignificant improvement in gastrointestinal symptoms[iii]. In fact, there may be other mechanisms at play within the duodenum that cause steatorrhea and contribute to low duodenal pH, namely inadequate bile secretion, possibly due to a diet low in bitter plant constituents. Here, I will discuss the issue of gastroesophageal reflux disease (GERD) in CF and the negative consequences of using PPIs to treat it. I will also discuss the many negative side effects of long term PPI use in the CF and general populations. In addition, I will discuss the low bicarbonate theory in its relationship to pancreatic enzyme activation, and how the use of PPIs may not be helpful in this situation. Lastly, I will discuss the role of bitter plant constituents in stimulating release of GI hormones and bile in the duodenum, their relationships to macronutrient absorption, and how the use of bitter tastants in the CF population may kill two birds with one stone: addressing GERD by correcting gastric sphincter function and GI secretions, and improving lipase activation by stimulating release of bile which emulsifies fats and stimulates bicarbonate secretion. |
Author
Mica (they/he) is a clinical herbalist, nutritionist, researcher, and writer living in Abenaki territory (Vermont). *************************** Disclaimer: The content of this website and blog is for educational purposes only and should not be considered medical advice. The information provided here is not intended to replace medical care. Archives
July 2024
Categories
All
|
Photo from BotanikGuide

 RSS Feed
RSS Feed
